Abstract
Introduction
Phosphatidylinositol-3-kinase (PI3K) inhibition has emerged as a novel targeted mechanism for achieving durable remission in CLL in both the untreated and relapsed/refractory setting. Despite this profound efficacy, PI3K inhibition with the delta isoform inhibitor, idelalisib, has been linked with significant autoimmune toxicity including hepatitis and colitis. Treatment naïve patients receiving idelalisib with ofatumumab in a phase 2 trial had high rates of autoimmune hepatitis within the first month of treatment (Lampson, Blood, 2016). We have previously shown that a reduction in CD4+ regulatory T cells (Tregs) likely predisposes to this toxicity. Here we report additional details of T cell populations observed in these idelalisib-treated patients, with and without severe toxicity.
Methods
To better characterize the immunologic mechanism of this toxicity, we evaluated samples from study participants using single cell mass cytometry (CyTOF) with a panel of 26 surface membrane and 9 intracellular markers focused on T cell populations (Lampson et al). CyTOF was performed on 26 peripheral blood mononuclear cell (PBMC) samples from 14 patients, at baseline and one month on therapy, the timepoint of autoimmune hepatitis. Flow cytometry standard (fcs) files were processed using FlowJo to gate on viable, singlet cells. The CD3+ events from each sample were exported as individual fcs files to Cytobank.org for analysis.
Patients were analyzed in two groups: absent or mild hepatitis (grades 0,1, and 2) vs severe hepatitis (grades 3 and 4) as defined by CTCAEv4.0. viSNE was used to visualize high-dimensional CyTOF data and identify islands for validation (Amir, Nature Biotechnology, 2013). We confirmed these findings by isolating cell populations as percentages of total CD4+ T cells.
Results
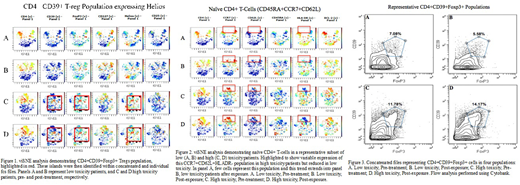
Our analysis of four individual groups demonstrated that CD4+ T cells as a percentage of CD3+ T cells were greater in high toxicity patients than in low toxicity, at baseline and one month, but without significant change during therapy (62.5 vs. 48.2 at baseline; n=9 and n=4, respectively). Evaluation of Tregs showed significant decrease following idelalisib exposure. This was seen when defining Treg cells as CD4+CD25+CD127- as well as when adding Foxp3 expression. viSNE analysis further identified discrete populations.
CD4+CD39+Foxp3+ Tregs
This is a Treg subset that expresses CD39 and Helios (Figure 1). Across timepoint and toxicity, it is more than two-fold higher in patients with high toxicity, representing 9.6% of CD4+ cells in high toxicity compared with 4.1% in low toxicity. After one cycle of treatment, these percentages declined to 7.5% and 3.2%, respectively.
Further, CD39 is expressed by 67% of all Treg cells in this cohort and has been previously suggested to associate with autoimmune response (Zhao, Frontiers in Immunology, 2017). A relative decrease is observed in all patients after exposure, but the reduction of CD39 expressing Treg cells is more robust in low toxicity patients.
Naïve CD4+ T Cell: CD62L+CCR7+CD45RA+HLA-DR-
The population of naïve T cells is present at baseline in low and high toxicity patients, 5.4% and 10.5% of CD4+ cells, respectively (Figure 2). After one month of exposure to idelalisib, this population in high toxicity patients increased to 14% but remained the same in low toxicity.
Conclusion
This CyTOF analysis among patients with and without severe autoimmune hepatic toxicity on idelalisib demonstrates relative expansion of CD4 populations in patients who developed toxicity. We identify two CD4 T cell subsets in patients experiencing severe hepatotoxicity. The CD4+CD39+ Treg population emerges as a leading candidate for further evaluation. In leukemic cells, CD39 has been reported to promote differentiation of specific Tregs (Vaisitti, International Journal of Molecular Sciences, 2018). Furthermore, CD39 expression on T-cells has been shown to confer worse outcomes in CLL (Perry, Annals of Hematology, 2012). The mechanism for this remains unknown.The second population is a subset of naïve T cells that grows following treatment only in high toxicity patients.
An expanded cohort from this trial is currently being analyzed with an updated T cell focused CyTOF panel to further evaluate these findings. If validated, CD39 expressing T cells may help predict susceptibility to severe autoimmune mediated hepatotoxicity prior to PI3K-based treatment of CLL.
Brown:TG Therapeutics: Consultancy; Verastem: Consultancy, Research Funding; Beigene: Membership on an entity's Board of Directors or advisory committees; Acerta / Astra-Zeneca: Membership on an entity's Board of Directors or advisory committees; Morphosys: Membership on an entity's Board of Directors or advisory committees; Loxo: Consultancy; Sunesis: Consultancy; Sun Pharmaceutical Industries: Research Funding; Roche/Genentech: Consultancy; Genentech: Consultancy; Boehringer: Consultancy; Pharmacyclics: Consultancy; Janssen: Consultancy; Celgene: Consultancy; Invectys: Membership on an entity's Board of Directors or advisory committees; Gilead: Consultancy, Research Funding; Abbvie: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal